Scleroderma
Scleroderma is an autoimmune disorder of the connective tissues where the body's immune system mistakenly attacks its own cells. Scleroderma is characterized by hardening of the skin, scar formation (fibrosis), blood vessel disease and inflammation associated with an over active immune system. The disease usually affects people between the ages of 30-50 years with women more prone to the condition than men.
Types of Scleroderma.
Scleroderma can be classified based on the location and involvement of internal organs into two types:
Localized scleroderma
Systemic scleroderma
Localized scleroderma involves skin changes in isolated areas, either as morphea patches or linear scleroderma. Morphea is localized patchy areas of skin that become hard and slightly pigmented and can sometimes cause multiple lesions on the skin. Linear scleroderma is more common in children and features bands of hardened skin localized usually to the arm or leg on one side of the body. Localized Scleroderma is the milder form of the disease and will not progress to Systemic scleroderma, a more severe form.
Systemic scleroderma affects connective tissues of the skin and also that of the internal organs such as the heart, lungs, kidneys and digestive tract. The tissues of the affected organs may become hard and fibrous decreasing their efficiency. Systemic Scleroderma is also further categorized as Limited or Diffuse:
Limited disease: This is a slower and more benign illness, typically confined to the fingers, hands, and face. It is also referred to as CREST syndrome which stands for Calcinosis, Raynaud phenomenon, Esophageal dysfunction, Sclerodactyly, and Telangiectasia.
Diffuse disease: This type presents with rapid skin thickening progressing to skin hardening and a high risk of developing fibrous hardening of the internal organs including the lungs, heart, bowels, esophagus and kidneys. Diffuse disease is a very serious form and can ultimately be fatal.
Causes and risk factors.
The cause of scleroderma is unknown.
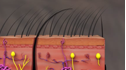
Research studies indicate certain inherited genes may be responsible along with exposure to environmental factors such as silica dust and paint thinners or exposure to certain viruses. It is known that people with Scleroderma develop extra collagen in the skin and organs which leads to the symptoms associated with the disease.
Symptoms.
The symptoms depend upon the type of scleroderma and which organs are affected such as the skin, heart, lungs, kidneys, and digestive tract. Commonly seen symptoms of scleroderma include:
Thick, tight skin on the fingers
Sores (ulcers) on the fingertips or toes
Hair loss
Red spots on the hands and face
Pain, stiffness, and swelling of the fingers and joints
Calcium deposits in connective tissues
Joint pain
Raynaud’s phenomenon. narrowing of blood vessels in the hands or feet
Swelling of the esophagus, the tube between your throat and stomach
Constipation or diarrhea
Shortness of breath
Dry cough and wheezing
Diagnosis.
Scleroderma may be diagnosed through the following tests:
Blood tests: To assess elevated levels of certain antibodies produced by the immune system
Tissue sample: A biopsy of the affected skin is taken for examination in the laboratory
Skin assessment: This involves a thorough evaluation of the skin to assess for clues of involvement of the internal organs.
Depending upon the condition of the patient and the results of the initial evaluation the doctor may recommend further specific diagnostic tests.
These tests may include chest X-rays, lung-function test, CAT scan of the lungs, EKG and echocardiograms.
Treatment.
There is no cure for scleroderma but rather symptoms are controlled through medications such as immunosuppressants, corticosteroids, vasodilators, and blood pressure medications.
The skin lesions associated with scleroderma can be camouflaged through cosmetic procedures such as exposure to ultraviolet light or laser surgery.
Physical or occupational therapy may be recommended to manage pain and to improve your strength and mobility.
In some cases, such as finger ulcers in severe Raynaud’s disease, surgical amputation may be recommended. Similarly patients with severe pulmonary hypertension may require lung transplants.
Patients with a mild form of scleroderma may not require any treatment.
Complications.
Possible complications related to scleroderma are as follows:
Heart failure
Pulmonary hypertension
Cancer
Kidney failure from elevated blood pressure
Esophageal stricture
Malabsorption of food nutrients
Pulmonary Fibrosis (scarring of the lungs)
Scleroderma is an autoimmune disorder of the connective tissues, characterized by hardening of the skin, and scar formation.